Background: Sickle cell disease (SCD) is a complex inherited blood disorder associated with high acute healthcare utilization, further complicated by psychosocial and socioeconomic factors. Social determinants of health (SDOH) have a known impact on healthcare access and health outcomes, particularly in minoritized communities. The Area Deprivation Index (ADI) is a composite measure of neighborhood socioeconomic disadvantage. The Childhood Opportunity Index (COI) is a validated approach for estimating multi-dimensional SDOH leading to inequitable distribution of opportunity across neighborhoods. Both have been associated with acute care utilization in pediatric populations other than SCD. We hypothesize that ADI and COI will be associated with acute care utilization and care access in SCD, as well.
Methods: Data were collected retrospectively from the electronic medical record between September 2021 and July 2023 for patients followed at a Midwestern Pediatric SCD Clinic who completed a Psychosocial Assessment Tool (PAT) at an annual comprehensive visit. The PAT is a validated quantitative caregiver survey used to screen for psychosocial risk factors and resiliency, with subcategories such as social support, child problems, structure/resources, and family beliefs. Number of emergency department (ED) visits, hospitalizations, and missed clinic visits were collected from the time the PAT was completed up to 1 year after (or the end of the data collection period). The area deprivation index (ADI) and childhood opportunity index (COI) were determined utilizing census block data for the patient at the time the PAT was completed. Descriptive statistics were performed on all data above, as well as t-tests and chi square tests for univariate analyses.
Results: One hundred seventy-four unique patients completed a PAT during the study period. The median age of the child with SCD was 11.5 years (range 4-22 years), with the majority having Hb SS disease (61%). Eighty-nine percent had a primary care provider documented and 75% had public insurance.
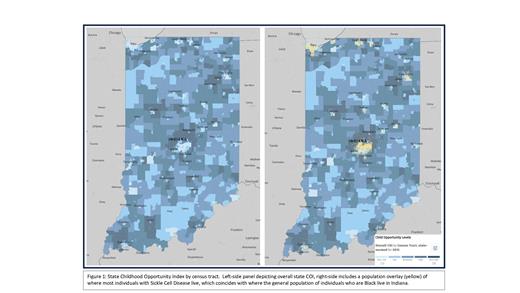
The median state ADI (6) and COI (2) for the cohort demonstrated significant neighborhood disadvantage/SDOH for all patients (See Figure). Ninety-two unique patients had 239 ED encounters. Fifty-eight unique patients accounted for 149 hospitalizations. Forty-seven percent of those hospitalized had a PAT in the Targeted or Clinical range (i.e. increased psychosocial stressors) compared to 30% of those who had not been hospitalized ( p=0.04).
There was no statistically significant difference between ADI or COI and number of ED encounters or hospitalizations. However, patients who missed 1 or more SCD visits (n=79) had a higher median state ADI than those who did not miss a visit (8 vs 6, p=0.009). Median state COI was also lower in this group than those who did not miss a visit (1 vs 2, p=0.008). Forty-eight percent of those who missed 1 or more SCD visit had a PAT in the Targeted or Clinical category versus 27% of those who did not miss any ( p=0.009).
Conclusion: While those with significant SDOH and neighborhood disadvantage did not have higher rates of acute care utilization in this cohort, there was a significant contribution to missed preventative SCD care visits, further emphasizing the need for psychosocial support and resources as essential elements to SCD programs, as well as alternative forms of care delivery, such as telemedicine, to improve access to SCD specialists. Further studies are needed to understand the impact comprehensive resources such as these may have on care burden, as well as disease outcomes.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal